What is Dry Eye Syndrome?

What is Dry Eye?
Causes of Dry Eye
-
Aging
Tear production inherently declines with age, contributing to the higher prevalence of dry eye in older persons.
-
Medical Conditions
Sjogren's syndrome, diabetes, lupus, rheumatoid arthritis, and thyroid issues can all aggravate dry eye.
-
Medication
Antihistamines, decongestants, blood pressure pills, antidepressants, and acne drugs like isotretinoin can cause a decline in tear production.
-
Environmental factors
Tear evaporation can be exacerbated by exposure to smoke, wind, dry regions, high altitudes, and even air pollution, which can result in dry eyes.
-
Extended Screen Time
Staring at computer screens, cellphone screens, or other digital gadgets for a longer period might cause blinking and tear production to decrease.
-
Contact Lenses
Wearing contact lenses for longer periods can disrupt the tear film's normal composition, exacerbating symptoms of dry eyes.
-
Hormonal Changes
Tear production can be impacted by hormonal fluctuations, especially in women who are pregnant, menopausal, or using oral contraceptives.
-
Eyelid Issues
Dry eyes can result from conditions such as blepharitis (inflammation of the eyelids), entropion (inward turning of the eyelids), or ectropion (outward turning of the eyelids).
-
Eye Surgery
The temporary reduction in tear production following procedures like LASIK or cataract surgery might exacerbate dry eye syndrome.
-
Vitamin A Deficiency
Lack of Vitamin A can cause dry eyes which is necessary for good eyesight.
-
Meibomian Gland Dysfunction (MGD)
Dry eyes and low-quality tears can be caused by gland dysfunction that affects the production of the greasy component of tears.
-
Autoimmune disorders
Sjogren's syndrome and other similar conditions drastically reduce tear output by particularly targeting the glands that produce tears.
-
Allergies
Inflammation brought on by allergic reactions might impact the stability and production of tears.
-
Diet and Nutrition
An imbalanced diet and a lack of omega-3 fatty acids can have an impact on the quantity and quality of tears produced.
-
Dehydration
Drinking too little water might cause the eyes to produce fewer tears, leaving them dry.
-
Sleep Apnea
Because of air leaking around the mask, using CPAP devices for sleep apnea can increase the risk of dry eyes.
-
Use of Preservatives in Eye Drops
Using eye drops containing preservatives on a regular basis might aggravate dry eye symptoms and cause irritation to the eyes.
-
Radiation Therapy
Radiation therapies for cancer, especially those that involve the head and neck, might harm tear glands and cause dry eyes.
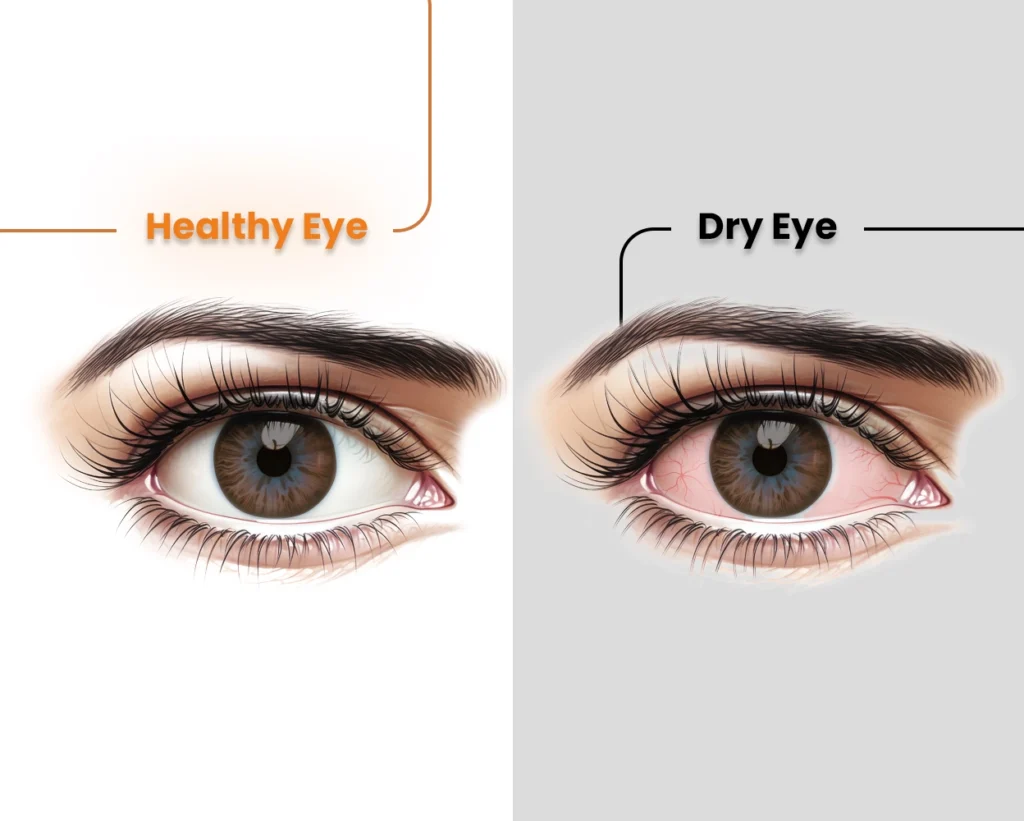
Symptoms and Diagnosis of Dry Eye
Stinging or Burning Sensations
Scratchiness
Redness
Sensitivity to Light (Photophobia)
Watery Eyes
Blurry Vision
Eye Fatigue
Difficulty Wearing Contact Lenses
Stringy Mucus
Heavy Eyelids
Difficulty with Night Vision
Foreign Body Sensation
Excessive Eye Watering
Discomfort with Wind or Air
Increased Blinking
Pain and Soreness
Eye Strain
Difficulty Reading or Focusing
Halos Around Lights
Diagnostic Procedures for Dry Eye Disease
- Patient History and Symptom Evaluation: This involves asking the patient about their symptoms, medical history, medication use, and lifestyle factors that might contribute to dry eye.
- Schirmer Test (to measure tear production): This test will diagnose whether your eyes produce enough tears to maintain moisture. A filter paper is placed inside the lower eyelid. After 5 mins, the moisture content is measured on the paper. Tear Breakup Time (TBUT) Test: This test evaluates the stability of the tear film. Fluorescein dye is instilled into the eye, and the time it takes for dry spots to appear on the corneal surface is measured.
- Ocular Surface Staining: Dyes such as fluorescein, lissamine green, or rose bengal are used to stain the ocular surface, helping to identify areas of damage or dryness.
- Tear Osmolarity Test: This test measures the concentration of solutes in the tear film, with higher osmolarity indicating dry eye.
- Meibomian Gland Evaluation: This involves examining the eyelid margins and meibomian glands to check for blockages or dysfunction, which can contribute to dry eye.
- IDRA (Integrated Diagnostic for Dry Eye):
- Tear Film Analysis: IDRA provides a comprehensive analysis of the tear film, including its lipid, aqueous, and mucin layers.
- Meibography: This non-invasive imaging technique visualizes the meibomian glands, assessing their structure and function.
- Non-Invasive Tear Break-Up Time (NIBUT): Measures the stability of the tear film without the need for dyes.
- Tear Meniscus Height Measurement: Evaluates the quantity of the tear film.
- Blink Analysis: Assesses blink patterns and completeness, which can affect tear distribution and ocular surface health.
- Ocular Surface Staining: High-definition imaging detects surface damage and dryness.
- TearLab Osmolarity System: Measures the osmolarity of tears, providing an objective metric of tear film health and stability.
- InflammaDry Test: Detects elevated levels of matrix metalloproteinase-9 (MMP-9), an inflammatory marker often increased in dry eye disease.
- LipiView and LipiScan: These devices provide high-resolution imaging of the tear film and meibomian glands, allowing for detailed assessment of lipid layer thickness and gland structure.
- Oculus Keratograph 5M: Offers comprehensive dry eye analysis, including non-invasive tear break-up time, tear meniscus height measurement, meibography, and infrared imaging of the meibomian glands.
- Spectral-Domain Optical Coherence Tomography (SD-OCT): Used to image the tear meniscus and measure tear volume.
- Confocal Microscopy: Provides detailed images of the corneal surface and sub-basal nerve plexus, which can be affected in dry eye disease.
- Corneal Topography: Maps the curvature of the cornea, which can be altered in dry eye disease, affecting vision.
Book Your Consultation for Dry Eye Treatment!
Dry Eye Treatment Options
- Artificial Tears and Lubricating Eye Drops: These relieve symptoms by reducing irritation and inflammation while adding moisture. This method provides temporary relief in dry eye disease treatment.
- Lifestyle Changes (e.g., reducing screen time, using humidifiers): Taking time off-screen minimizes eye strain and dryness. Humidifiers add moisture to the air, preventing the eyes from drying out. These changes can help ease dry eye symptoms naturally.
- Warm Compresses and Eyelid Scrubs: These offer gentle and natural relief from eye irritation and redness. Use a clean washcloth moistened with warm water. Check the temperature of the cloth before placing it on your eyelids for 2 minutes. This helps remove crusty debris from the lashes and loosens oil in the meibomian glands.
- Omega-3 Fatty Acid Supplements: As a trusted source in your search for a “dry eye specialist near me,” we recommend Omega-3 supplements. Found in fish oil, these enhance the quality of tear production and maintain a healthy tear film. Regular intake of Omega-3s improves eye comfort and reduces dryness.
- Prescription Medications (e.g., anti-inflammatory eye drops): These drops target the underlying cause of inflammation, promoting relief and maintaining a healthy tear film. It’s an effective way to receive a dry eye treatment.
- Punctal Plugs (to conserve tears) Tiny silicone plugs help block tear ducts, shutting the small openings in the inner corners of the eyelids. This method conserves both natural and artificial tears.
- LipiFlow (thermal pulsation treatment for meibomian gland dysfunction) This FDA-approved dry eye disease treatment addresses meibomian gland dysfunction, a leading cause of dry eye. LipiFlow treats the eyelids by massaging and warming their insides, helping to restore healthy oil production and enhance tear quality.
- Intense Pulsed Light (IPL) Therapy IPL therapy is a new method for treating evaporative dry eye and rosacea. Oxyhemoglobin absorbs the light spectrum from the flash lamp, causing heat-induced ablation of vascular structures.
- Autologous Serum Eye Drops (using the patient’s blood components) The biochemical components in autologous serum eye drops resemble natural tears. Unlike artificial ones, they reduce inflammation and provide eye relief, offering one of the best treatments for dry eye.
- Cyclosporine Ophthalmic Emulsion: Research has shown that this medication can increase tear production in patients with dry eye disease caused by inflammation.
- Lifitegrast Ophthalmic Solution: This relatively new treatment option works by inhibiting inflammation, providing relief from dry eye symptoms.
- Amniotic Membrane Extract Drops: Recent studies suggest that drops made from amniotic membrane extract can help heal the ocular surface and reduce inflammation in patients with severe dry eye.
- Microblepharoexfoliation (MBE): This innovative procedure exfoliates the eyelid margins to remove biofilm and debris, improving the function of the meibomian glands and relieving dry eye symptoms.
- Low-Level Light Therapy (LLLT) New research indicates that LLLT can improve meibomian gland function and tear stability, offering relief for patients with evaporative dry eye.
Consultation with experienced specialists, such as those at Shri Venkatesh Eye Institute, can provide personalized guidance and insights into best dry eye treatment options for your needs.

Why Our Dry Eye Specialists are the Best Choice for Your Care?
Specializing in offering dry eye treatment in Mumbai, Shri Venkatesh Eye Institute as a dry eye clinic offers unparalleled expertise in delivering exceptional care to its patients. Imparting accurate and transparent information is our goal and you will find it here as you skim through “dry eye specialist near me” over the web. Modern scanning tools focus on patient safety besides being affordable for those who don’t want to compromise on quality.
Choosing Shri Venkatesh Eye Institute means receiving comprehensive treatment from our dry eye specialists at an affordable cost. Both our non-surgical and advanced treatments show results in no time.
